Peripheral vascular disease
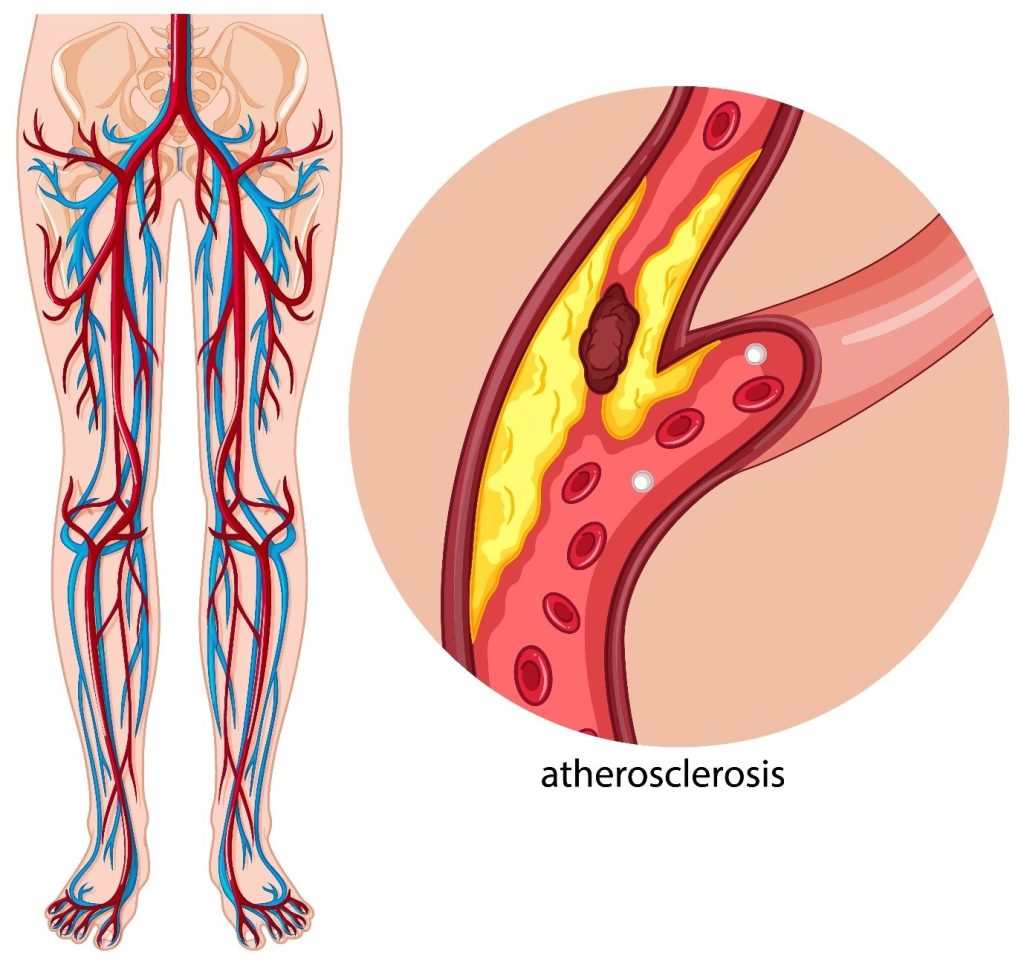
Peripheral vascular disease (PVD) is a circulatory disorder that causes the blood vessels outside the brain and heart to narrow.
By Admin | 16 February 2024What is peripheral vascular disease?
Peripheral vascular disease (PVD) is a circulatory disorder that causes the blood vessels outside the brain and heart to narrow. This can happen in arteries as well as veins. The blood vessels get narrowed due hardening of the arteries (atherosclerosis) or due to spasm in the blood vessels.
PVD is also referred as:
- Claudication
- Arteriosclerosis obliterans
- Arterial insufficiency
- Intermittent claudication
What are the risk factors for PVD?
- Elevated serum cholesterol
- Smoking
- Hypertension
- Obesity
- Diabetes
- Family history of stroke
Peripheral Arterial Disease (PAD)
Peripheral arterial disease occurs in only arteries. PAD is the most common form of PVD, so the terms are often used to mean the same condition.
ARTERIAL DISORDERS
1) Acute arterial occlusion-
- A thrombus, embolism, or trauma can cause acute loss of blood flow to peripheral arteries. It’s a medical emergency condition.
2) Arteriosclerosis Obliterans
- This accounts for 95% of all the arterial disorders, and it affects mainly the lower extremities. Mostly seen in large or medium sized arteries of lower limb. Occurrence is more prevalent in males than females.
3) Buerger’s Disease
- It is a specific disease entity affecting small and medium sized arteries and veins of the extremities and characterized by acute or chronic occlusive inflammatory involvement. More common in men under the age of 35 years who are chain smokers.
- Clinical features of buergers disease are:
- Pain or tenderness
- Enlarged, red, tender cord like veins
- Numbness and tingling in limbs
- Skin ulcers
- Gangrene in digits
- Pain with activity like walking and decreases with rest.
4) Raynaud’s disease
- It is generally seen in women with some abnormality in the sympathetic nervous system. It is characterized by digital vasospasm and affects the small arteries of fingers and toes.
- The aggravating factor is cold, vibration, or stress.
- The response to this is temporary pallor, cyanosis and pain, numbness and cold sensation of digits.
- However, clinically there would be diminished or absent peripheral pulses, integumentary changes, sensory disturbances and intermittent claudication.
COMPLICATIONS OF PVD
- There are various complications such as tissue death leading to amputation, pallor skin, severe pain that restricts mobility, unhealed wounds, infections of bones and blood stream.
- The severe complications can lead to heart attack, brain stroke or death.
DIAGNOSIS OF PVD
- Early diagnosis if the initial step to successful treatment and can prevent life threatening complications. The examination includes the following-
- Palpation and comparison of pulses in the involved and uninvolved upper or lower extremities.
- Skin temperature
- Skin integrity and pigmentation
- Tests for reactive hyperemia
- Claudication time
- Ultrasonography, Doppler measurement of blood flow
- Transcutaneous oximetry
- Magnetic resonance angiography
- Arteriography
PREVENTION OF PVD
- PVD can be prevented through a healthy lifestyle which includes avoiding smoking, controlling blood sugar levels, lowering cholesterol, eating a healthy diet, maintaining optimal blood pressure levels, exercising for at least 30 minutes a day and 5 times a week and keeping an eye on increasing weight.
TREATMENT OF PVD
- The main goal of PVD is to stop the disease from progressing and to alleviate pain and manage the symptoms. The first line of treatment involves lifestyle modifications that includes a well-balanced diet, a regular exercise regimen and to stop addictions like smoking. Medical management includes certain drugs like cilostazol, clopidogrel, aspirin, atorvastatin, ACE- inhibitors.
- Severely, blocked arteries require surgical intervention like angioplasty or vascular surgery.
- Certain exercise protocols like Buerger- allen exercise can be followed.






